According to the World Health Organization (WHO), between 250,000 and 500,000 people suffer from spinal cord injuries (SCIs) every year due to blunt force trauma, road crashes, falls, and other mechanisms of injury. [1] A few years ago, this would have meant the end of autonomy and mobility for many people, but thanks to advances in technology, there are more rehabilitation therapies available, including exoskeletons. The FDA designates medical exoskeletons as a class II (intermediate risk) medical device, and they are cleared for use with patients who have an SCI. [2]
Exoskeletons give people with spinal cord injuries a chance to ambulate, exercise, and engage in mobility and autonomous activities. In this article, you’ll learn what exoskeletons are, how they operate, and how they can be beneficial in physical therapy for patients with spinal cord injuries.
What is a Spinal Cord Injury (SCI)?
According to the National Institute of Neurological Disorders and Stroke (NINDS), a spinal cord injury is “damage to the tight bundle of cells and nerves that sends and receives signals from the brain to and from the rest of the body.” [3] SCIs could be a direct result of damage to the spinal cord itself, such as from a gun shot wound, but could also result from damage to surrounding tissues and bones that then compress the spinal cord. These injuries can permanently or temporarily affect mobility, sensation, and other body processes. Depending on the extent and location of the damage to the spinal cord, patients may experience some form of paralysis and/or sensory deficits that could be improved through rehabilitation, potentially leading to full recovery.
The most common causes of SCI are grouped into traumatic and non-traumatic causes. Traumatic SCI causes may include car accidents, falls, and sports-related accidents. Non-traumatic causes include tumors, neurodegenerative diseases, infections, and genetic causes.
Rehabilitation Methods Available for Patients with Spinal Cord Injury

Rehabilitation therapies for patients with a spinal cord injury depend on the extent of damage and the type of injury. Patients usually start in the intensive care unit, followed by acute care, inpatient, and outpatient rehabilitation. Some hospitals even have a spinal cord injury department that specializes in this type of rehabilitation. This can last anywhere from three to twelve months or more, depending on the severity of the injury. Popular rehabilitative techniques include:
- Range of Movement, Strength, and Stretching Exercises
Spinal cord injuries limit the range of movement by causing joint immobility and flexibility issues. However, this can be remedied using stretching and strength exercises. According to a 2020 study, range of movement exercises help “prevent contractures, protect tenodesis effect, strengthen paralyzed muscles, promote nerve and cerebral remodeling, and improve spinal microenvironment and functional prognosis.” [3]
- Functional Electrical Stimulation
Functional electrical stimulation works by artificially stimulating the sensory-motor systems using electrical pulses. It activates neural pathways, which stimulate the muscles and cause movement. This therapy is used alongside other rehabilitation methods in order to restore mobility. According to a study, this procedure also “provides cardiorespiratory fitness; improves posture and trunk stability; prevents contractures, pressure ulcers, and orthostatic hypotension; promotes nerve restoration; and prevents peripheral nerve deterioration.” [4]
- Epidural Electrical Stimulation (EES) of the Spinal Cord
In this procedure, a device is implanted over the spinal cord’s dura mater through a laminectomy. It then produces a rhythmic electric pulse to the posterior nerve roots, which activate the central circuits which are responsible for regulating pain, movement, and the cardiorespiratory system. EES is beneficial for reducing fatigue, improving cardiovascular fitness, increasing body mass, and improving urination in patients. [4] However, this is not a simple procedure, as patients must undergo surgery for the device to be implanted and is not yet widely available.
- Transcutaneous Electrical Nerve Stimulation (TENS)
TENS utilizes a high and low electrical stimulation to the nerve to manage pain. It may also help with proprioception, balance, and spasticity. This method is very affordable, and patients can do it by themselves without much assistance.
- Occupational Therapy
Occupational therapy focuses on improving the physical, sensory, and cognitive functions of the patients. It helps patients suffering from SCI regain their autonomy and independence. It focuses on the execution of daily activities like grooming, bathing, cooking, and dressing, among others. Occupation is the gateway that helps patients attain inclusion and total adaptation to their environment.
- Robotic Exoskeletons
Wearable robotics, also known as robotic exoskeletons or exosuits, are a recent development in the healthcare industry that present unlimited potential for patients with spinal cord injuries and are used in conjunction with physical therapists. Robotic exoskeletons are used in rehabilitation to help in mobility recovery through repeated movements that lead to increased neural plasticity. [5] Exosuits offer benefits like improved gait, better life quality, improved moods, and better bladder control, among others, as discussed below.
According to Dr. Chester Ho, Associate Professor at the University of Calgary’s Department of Clinical Neurosciences and member of the Hotchkiss Brain Institute, introducing robotic exosuits early in a patient’s rehabilitation process offers better chances of recovery. He says, “The first nine months after a spinal cord injury are pivotal to recovery, so we want to attempt to introduce rehabilitation and mobilization early on and see if it makes a difference.” [6]
What Is An Exoskeleton?
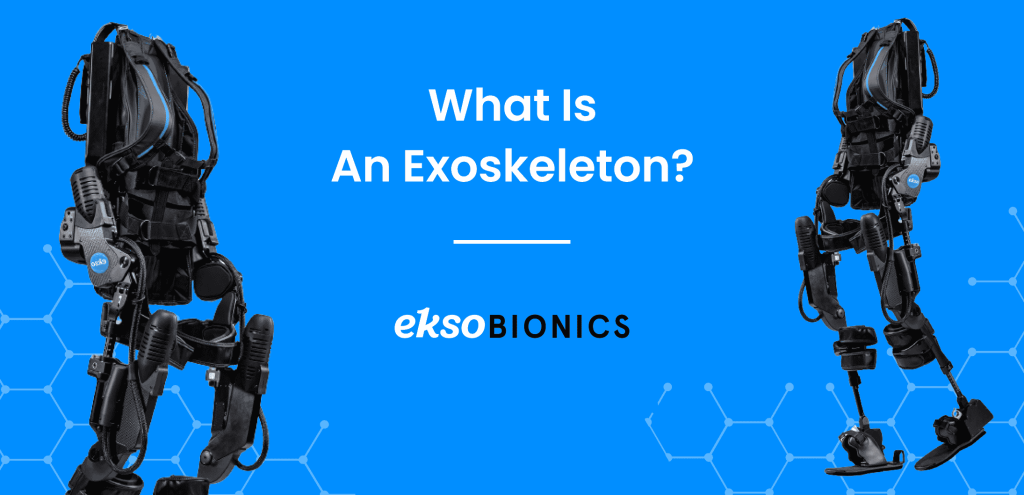
Exoskeletons, first developed in 1890, are wearable electromechanical devices that support joint movement while enhancing the wearer’s strength and ambulatory capabilities. An exoskeleton frame is made to surround the waist and other joints like the shoulders and knees. Exoskeletons can be classified into two types: active, powered by an external power source; or passive, powered by mechanical springs and counterbalance forces.
Exoskeletons are used in physical rehabilitation clinics to promote a patient’s mobility and increase their muscle strength. They do this by allowing for repeated movements that increase neural plasticity and help develop mobility. [4] The use of exoskeletons in physical therapy is reported to increase “quality of life, body composition, bone density, neuropathic pain, spasticity, gait speed, number of steps, and distance before and after 90 days of training.” [4]
How Are Exoskeletons Controlled?

Exoskeleton control is vital in a physical therapy environment. Exoskeletons offer multiple control modes, and operators can choose the amount of resistance that is applied at the joints. Exoskeletons can be controlled by the patient or physical therapist depending on the degree of patient recovery. Control methods include: [7]
- Sensors: Sensor-controlled exosuits have numerous sensors fitted into the build that capture nerve signals and control torque, pressure, tilt, and rotation.
- Buttons/control panels: Some exosuits contain pre-programmed modes, which are normally controlled by the user or by the physical therapist. Most control panels are located on the walking aids.
- Joystick: This is commonly found in active exosuits that provide all the energy required by the wearer.
- Mind-Controlled: These use an electrode skull cap as the main method of control.
No-control: Most passive exosuits do not have control buttons and respond to the mechanical movements of the wearer.
Exoskeleton control is vital in a physical therapy environment. Exoskeletons offer multiple control modes, and operators can choose the amount of resistance that is applied at the joints. Exoskeletons can be controlled by the patient or physical therapist depending on the degree of patient recovery. Control methods include: [7]
- Sensors: Sensor-controlled exosuits have numerous sensors fitted into the build that capture nerve signals and control torque, pressure, tilt, and rotation.
- Buttons/control panels: Some exosuits contain pre-programmed modes, which are normally controlled by the user or by the physical therapist. Most control panels are located on the walking aids.
- Joystick: This is commonly found in active exosuits that provide all the energy required by the wearer.
- Mind-Controlled: These use an electrode skull cap as the main method of control.
No-control: Most passive exosuits do not have control buttons and respond to the mechanical movements of the wearer.
Types of Medical Exoskeletons

All exoskeletons are not built equally. They have different features and capabilities. In addition, the use of medical exoskeletons may differ between individuals based on the extent of injury and their recovery capacity. Exoskeletons are normally divided into:
- Upper Body Exoskeletons
Upper body exoskeletons are built to support the upper extremities, including the arms and torso. They are specifically designed to help patients with upper-body motor rehabilitation by positioning the shoulder, arm, and elbow through specific motions and orientations. They are extremely important to therapists because they can be used for intense motor exercises and task-specific movements.
- Lower Body Exoskeletons
Rehabilitative lower body exoskeletons are made for patients with lower limb motor dysfunctions to enable the recovery of lower extremity mobility. They normally use impedance control to generate resistance forces which are essential for rehabilitation training. Lower body exoskeletons have the ability to control joint movement in the hip, knee, and ankle.
Benefits of Using Exoskeletons After Spinal Cord Injuries

Exoskeletons are advantageous for patients and therapists alike. They have the ability to reduce the burden on therapists and help with quantitative data collection and patient evaluation.
- Gait Training:
Gait training consists of walking practice with the aim of helping the patient regain their normal walking gait. Using exoskeletons has the potential to make gait training easier and more convenient for therapists, given the numerous support features they offer. For instance, free-standing exoskeletons help patients to exercise in upright positions, which would be almost impossible and cumbersome without the use of exoskeletons. [8]
A 2008 gait training study carried out on two stroke survivors reports that “by the end of the training the gait pattern of the patients improved and became closer to a healthy subject’s gait pattern.” Improvement in this study was defined as “the increase in the size of the patients’ gait pattern, increased knee and ankle joint excursions and increase in their walking speeds on the treadmill.” [9] Exoskeletons also have unique features that help with rehabilitation. For example, the EksoNR has sensors that are made to monitor your patient’s leg movements and regulate their gait patterns. [10]
- Bladder and Bowel Function:
The use of exoskeletons may improve your patient’s bladder and bowel function. This is according to feedback that was received by researchers at the Spinal Cord Injury Model System Centers (SCIMS) from focus groups held with 30 therapists. They record that, “patients who gained the ability to stand and walk with an exoskeleton often developed better endurance, improved their bowel and bladder control, and were less likely to develop urinary tract infections.” [11]
Scientists believe that engaging patients in physical activities and maintaining upright postures may play a role in improving bowel motility. A 2019 study tested bowel management after exoskeleton training and reported an improvement of up to 80%. [12]
- Improved Muscle Strength and Spasticity:
Incorporating exoskeletons in your physiotherapy treatment may help patients improve their muscle strength. A 2021 study examining the effects of exoskeletons in physiotherapy observed that the use of exoskeletons improved grip strength, quadriceps strength, and lower limb motor function. [8] This was also observed in a 2019 study that reported exoskeletons improved muscle strength after a Manual Muscle Strength Test, “total score from both sides were: P3 UEMS increased from 30 to 37, and LEMS from 23 to 25; P11 UEMS increased from 33 to 37, and LEMS from 27 to 30, where the maximum score for UEMS and LEMS is 50.” [13]
Another study conducted on patients who had a stroke concluded that the use of exoskeletons in therapy improved the tibialis anterior muscle strength and lower limb motor function of the patients. [14]
- Improved Patient Moods:
Though not a significant benefit, the use of exoskeletons in therapy can help improve your patient’s moods. A 2021 study examining the effects of exoskeletons on patients with spinal cord injuries shows improved moods in one of the patients during the rehabilitation phase. It also reports a decrease in fatigue and an improved quality of life. [8] Since robotic exoskeletons are a “new” technology in rehabilitation, they can be exciting for patients and may motivate them to exercise more. Some therapists also report that exoskeletons offer extra psychological benefits to patients. For instance, patients reported psychological effects of having eye-to-eye conversations with others and also increased engagement in daily activities. [11]
- Patient Independence:
Exoskeletons can help patients gain some independence in their day-to-day activities like moving and walking around. Before the invention of medical exoskeletons, patients had to rely on their therapists to move around and exercise. However, that is no longer the case. They can now exercise and ambulate on their own, which gives them a sense of independence. Physical therapist Kyle McIntosh says, “The exoskeleton lets patients take actual steps, which is not only more realistic but much less cumbersome,” McIntosh also says, “Every step is different with this device, so patients learn from their mistakes in real time. Patients really like to use the device; it gives them hope.” [6]
Conclusion

Rehabilitative technology has come a long way, from crutches to walkers to wheelchairs and now, robotic exoskeletons. Robotic-assisted rehabilitation holds a lot of promise for both patients and physical therapists alike. Several studies have shown the potential benefits of exercising in a free-standing exoskeleton for patients with spinal cord injuries. If you are a physical therapist, this is the next medical technology shift that will help you offer next-level therapy solutions for your patients.
Ekso Bionics has been at the forefront of creating the best quality medical exoskeletons for more than a decade now. Our EksoNR was one of the first FDA-approved medical exoskeletons for rehabilitation, and it continues to be the exoskeleton of choice for many mobility rehabilitation clinics. Please review our indications for use to determine eligibility. [15]
References:
- Spinal cord injury https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury#:~:text=Key%20facts,traffic%20crashes%2C%20falls%20or%20violence. }
- Exoskeletal Assisted Rehabilitation After Spinal Cord Injury https://www.sciencedirect.com/topics/nursing-and-health-professions/exoskeleton-rehabilitation
- Spinal Cord Injury https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- Rehabilitation Therapies in Spinal Cord Injury Patients https://www.intechopen.com/chapters/72439
- Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review https://pubmed.ncbi.nlm.nih.gov/29987763/
- Spinal cord injury patients may benefit from using exoskeleton earlier in treatment https://ucalgary.ca/news/spinal-cord-injury-patients-may-benefit-using-exoskeleton-earlier-treatment
- Types And Classifications of Exoskeletons https://exoskeletonreport.com/2015/08/types-and-classifications-of-exoskeletons/
- Physiotherapy using a free-standing robotic exoskeleton for patients with spinal cord injury: a feasibility study https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-021-00967-4
- Robot Assisted Gait Training With Active Leg Exoskeleton (ALEX) https://ieeexplore.ieee.org/document/4663875
- https://backend.eksobionics.com/eksonr/
- Robotic Exoskeletons May Provide Health Benefits for People with Spinal Cord Injuriesnhttps://naric.com/?q=en/content/robotic-exoskeletons-may-provide-health-benefits-people-spinal-cord-injuries
- Changes in Bowel Function Following Exoskeletal-Assisted Walking in Persons with Spinal Cord Injury: An Observational Pilot Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7145720/
- Retraining walking over ground in a powered exoskeleton after spinal cord injury: a prospective cohort study to examine functional gains and neuroplasticity https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6868817/
- Impacts of a lower limb exoskeleton robot on the muscle strength of tibialis anterior muscle in stroke patients https://www.researchgate.net/publication/344023059_Impacts_of_a_lower_limb_exoskeleton_robot_on_the_muscle_strength_of_tibialis_anterior_muscle_in_stroke_patients/fulltext/5f519787a6fdcc9879c9cc2f/Impacts-of-a-lower-limb-exoskeleton-robot-on-the-muscle-strength-of-tibialis-anterior-muscle-in-stroke-patients.pdf
